Less Pain, Fewer Infections: How Vaginal Estradiol Hormone Therapy May Change Lives in Menopausal and Perimenopausal Women
Author: Quyen Johnson, APRN, FNP-C
Key Takeaways about Vaginal Estradiol and Women’s Health
- Vaginal estradiol is a well-researched, low-dose hormone therapy that offers targeted relief for common vaginal and urinary symptoms of menopause. For women with moderate to severe discomfort, it’s a safe and effective option backed by clinical evidence. Those with broader hormonal concerns may also consider Bioidentical Hormone Replacement Therapy (BHRT) as part of a more comprehensive, personalized care plan. Empowering yourself with knowledge and the right provider can make all the difference in navigating perimenopause and menopause with comfort and confidence.
1. Introduction about Declining Estrogen Levels
Menopause and perimenopause are natural parts of aging, but that doesn’t mean the changes they bring are easy to navigate, especially when it comes to vaginal and urinary health. For many women, symptoms like vaginal dryness, pain during intimacy, or frequent urinary tract infections begin slowly and quietly, but their impact can be anything but minor. These issues can affect everything from daily comfort to relationships and overall well-being.
What’s often behind these symptoms is something called Genitourinary Syndrome of Menopause (GSM), a common but frequently overlooked condition linked to lower estrogen levels. Many women assume it’s just something they have to live with, but the truth is that relief is possible.
Vaginal estradiol is one effective treatment option. It’s a low-dose, localized form of estrogen therapy that targets the root cause of GSM. Applied directly to the vaginal area, it helps replenish moisture, improve tissue health, and ease discomfort, without significantly altering hormone levels throughout the rest of the body.
In the sections ahead, we’ll break down how vaginal estradiol works, what the science says about its safety and results, and when it might be a good fit. For those curious about broader hormone support, we’ll briefly touch on how therapies like Bioidentical Hormone Replacement Therapy (BHRT) may complement care.
2. Common Symptoms Vaginal Estradiol Helps Relieve

Genitourinary Syndrome of Menopause (GSM) is the term supported by the International Society for the Study of Women’s Sexual Health (ISSWSH) and the North American Menopause Society (NAMS) to describe a group of symptoms affecting the vulvovaginal area, sexual function, and urinary tract due to reduced estrogen and other sex hormones after menopause.
Vulvovaginal Symptoms of Perimenopause and Menopause
These are the most commonly reported and include vaginal dryness, burning, irritation, reduced elasticity, and thinning of the vaginal and vulvar tissues. On examination, findings may show pallor, loss of vaginal folds (rugae), minor pinpoint bleeding (petechiae), and elevated vaginal pH. These tissue changes are progressive and typically do not resolve without treatment. [1–4]
Sexual Symptoms of Perimenopause and Menopause
GSM often causes painful intercourse (dyspareunia), reduced natural lubrication, and overall impaired sexual function. These symptoms may negatively affect both quality of life and intimate relationships. Women may also notice decreased arousal and difficulty with orgasm, often as a result of physical discomfort. [1–2][5]
Urinary Symptoms of Perimenopause and Menopause
Lower urinary tract issues are also common, including urgency, frequency, burning with urination (dysuria), and repeated urinary tract infections. Some women may develop stress or urge incontinence. These symptoms are linked to thinning and weakening of estrogen-sensitive tissues in the urethra and bladder trigone. [1–4][6]
Diagnosis is based on clinical presentation, specifically the presence of bothersome symptoms, while ruling out other causes. GSM affects up to 50% of postmenopausal women and remains underdiagnosed, in part due to hesitancy in discussing these symptoms. [1–5] Left untreated, GSM is a chronic and progressive condition, with symptoms that often persist or worsen over time. [3][7]
3. Vaginal Estradiol as a Therapeutic Intervention: Mechanism and Efficacy
Vaginal estradiol is a low-dose, localized estrogen therapy that targets estrogen receptors in the vaginal lining. By stimulating these receptors, it promotes the growth and maturation of the vaginal mucosa, helps restore a healthy balance of vaginal flora, increases the presence of mature superficial cells, reduces the number of immature parabasal cells, and reestablishes the vagina’s naturally acidic pH. These changes effectively reverse the thinning and inflammation associated with Genitourinary Syndrome of Menopause (GSM), leading to relief from vaginal dryness, painful intercourse (dyspareunia), irritation, and urinary symptoms [6, 8].

1. Clinical Effectiveness of Vaginal Estradiol
Robust evidence from randomized controlled trials and systematic reviews confirms the effectiveness of low-dose vaginal estradiol, typically administered at 4 to 25 micrograms daily for two weeks, followed by twice-weekly maintenance, for treating moderate to severe vulvovaginal symptoms like dryness, irritation, and pain during sex. Improvements in objective markers, such as vaginal cell health and pH levels, are consistently reported. Compared to placebo, vaginal estradiol provides marked symptom relief and measurable tissue regeneration, with minimal systemic absorption and a strong safety profile [9,10,11-13].
For women with mild symptoms, non-hormonal treatments like lubricants or moisturizers may offer comparable short-term relief. However, for those experiencing more persistent or multifaceted symptoms, vaginal estrogen tends to deliver more effective and lasting results [6,10,11-13].
2. Vaginal Estradiol and Recurrent UTIs
Building on established guideline recommendations, recent clinical trials and mechanistic studies have deepened our understanding of how vaginal estradiol impacts urinary tract infection (UTI) risk. Multiple randomized controlled trials and meta-analyses confirm that vaginal estradiol significantly lowers the incidence of recurrent UTIs in postmenopausal women, with relative risk reductions ranging from 36% to 75% compared to placebo, variations depending on formulation and study population. Notably, oral estrogen does not offer this protective effect and is not recommended for UTI prevention. [20-22]
Mechanistically, vaginal estradiol supports the restoration of the vaginal epithelium, reduces vaginal pH, and facilitates the recolonization of protective Lactobacillus species, key elements in lowering susceptibility to uropathogens [23]. In vitro and translational research further demonstrates that estradiol increases the expression of antimicrobial peptides and reinforces epithelial barrier function, providing a strong biological foundation for its clinical benefits [23,24]. Additionally, large retrospective cohort studies show a greater than 50% reduction in UTI frequency after initiating vaginal estrogen in hypoestrogenic women, with the most significant benefits seen in those with higher baseline UTI rates [5].
3. Guideline Recommendations for Vaginal Estradiol
Authorities such as the NAMS endorse vaginal estradiol as a first-line treatment for moderate to severe GSM when non-hormonal options fall short. [6]
The American Urological Association, alongside the Canadian Urological Association and the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction, recommends offering vaginal estrogen therapy to peri- and postmenopausal women with recurrent UTIs, as long as there are no contraindications to estrogen use. [19]
Given its low systemic absorption, additional progesterone is generally unnecessary to protect the uterine lining. Nevertheless, any postmenopausal vaginal bleeding should be promptly assessed by a healthcare provider. [6,12]
4. Safety Profile of Low-Dose Vaginal Estradiol
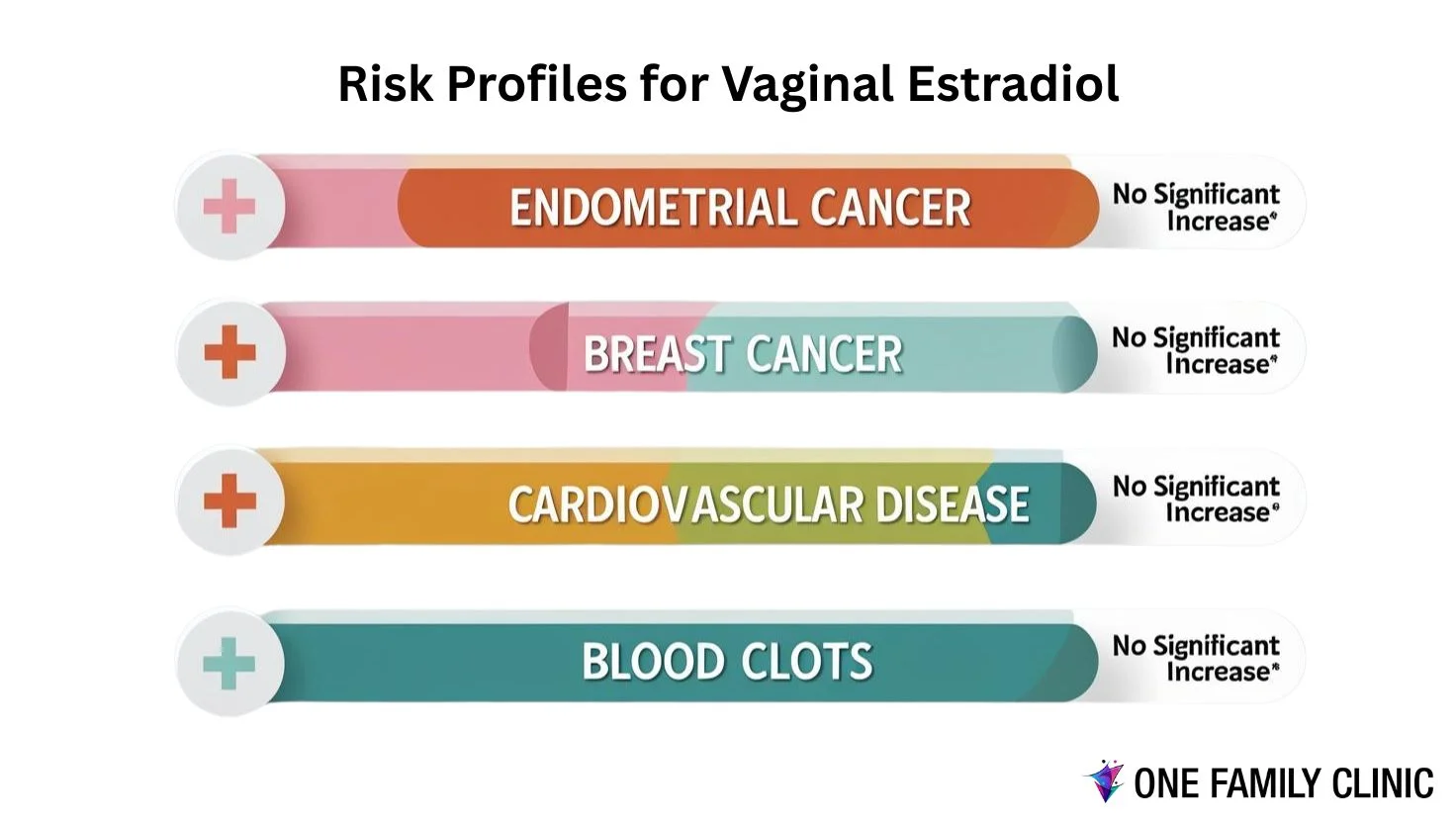
Low-dose vaginal estradiol has a well-established safety profile, marked by minimal systemic absorption and no clear evidence of increased risk for endometrial hyperplasia, endometrial cancer, breast cancer, cardiovascular disease, or venous thromboembolism in studies lasting up to one year. Randomized controlled trials and systematic reviews show that adverse effects are uncommon and comparable to placebo, with the most frequently reported side effects being headache, vaginal yeast infections (candidiasis), breast tenderness, and localized irritation [6, 7, 10, 14, 15, 16]
Endometrial safety is particularly well supported: multiple RCTs and systematic reviews have found no significant increase in endometrial hyperplasia or cancer with low-dose vaginal estradiol (e.g., 4–10 μg tablets or rings releasing ≤7.5 μg/day). In women with or without a uterus, progesterone is generally not required for endometrial protection when using these low-dose regimens. [6, 14, 15, 17]
Systemic estradiol levels remain within the expected postmenopausal range with these low-dose standard preparations, and observational studies show no increased risk of breast cancer recurrence or cardiovascular events, even among women with a history of breast cancer who are not taking aromatase inhibitors [6, 7, 17, 18]. The American College of Obstetricians and Gynecologists supports the use of low-dose vaginal estrogen as a reasonable option for women with a history of estrogen-dependent breast cancer. However, consultation with an oncologist is advised in more complex cases [18].
In summary, low-dose vaginal estradiol is generally well tolerated, with a safety profile similar to placebo over one year and no evidence of increased risk for serious estrogen-related adverse outcomes in the current body of research [6, 7, 15, 16].
5. Integrative Hormone Health and BHRT

While vaginal estradiol is a proven solution for relieving the localized symptoms of Genitourinary Syndrome of Menopause (GSM), many women experience broader hormonal shifts during menopause that affect more than just the vaginal and urinary systems. Common concerns such as hot flashes, night sweats, sleep disturbances, mood changes, and cognitive fog often emerge as estrogen, progesterone, and other hormone levels decline.
In these cases, a more holistic hormone support strategy may be beneficial. Bioidentical Hormone Replacement Therapy (BHRT) uses hormones that are molecularly identical to those naturally produced by the body. This approach allows individualized treatment plans based on a woman’s symptoms, lab values, and overall health goals.
While BHRT isn’t required for every woman using vaginal estradiol, it can be a meaningful option when symptoms extend beyond the scope of local treatment. Many healthcare providers take an integrative approach, including blending lifestyle modifications with personalized hormone therapy, to support physical and emotional well-being throughout the menopausal transition.
Clinics that offer BHRT often begin with a comprehensive assessment to determine whether systemic hormone therapy is appropriate and how it may complement treatments like vaginal estradiol. If you’re curious about this path, an informed discussion with a trusted healthcare provider is a valuable first step.
Summary
Perimenopause and menopause bring a range of physical and emotional changes, some expected, others more surprising or even isolating. Among the most common and treatable of these are vaginal symptoms such as dryness, discomfort, and urinary challenges. Vaginal estradiol offers a targeted, evidence-based solution that works locally to restore tissue integrity, ease discomfort, and improve overall quality of life.
With strong backing from clinical research and major medical guidelines, low-dose vaginal estradiol stands out as a practical option for women facing moderate to severe symptoms of Genitourinary Syndrome of Menopause (GSM). Non-hormonal treatments like moisturizers may offer sufficient relief for those with milder symptoms, while others may benefit from an integrative approach that includes broader hormone support.
Navigating this stage of life starts with understanding your choices. Whether you’re just beginning to notice changes or have been managing symptoms for a while, connecting with a knowledgeable, compassionate provider can help you feel empowered to make decisions that align with your health goals and overall well-being.
Bioidentical Hormone Replacement Therapy in Sherman, Texas and the Surrounding Areas
References
Portman DJ, Gass ML. Maturitas. 2014;79(3):349-54. doi:10.1016/j.maturitas.2014.07.013.
Portman DJ, Gass ML. The Journal of Sexual Medicine. 2014;11(12):2865-72. doi:10.1111/jsm.12686.
3. The Genitourinary Syndrome of Menopause.
Phillips NA, Bachmann GA. Menopause (New York, N.Y.). 2021;28(5):579-588. doi:10.1097/GME.0000000000001728.
4. Genitourinary Syndrome of Menopause: Management Strategies for the Clinician.
Faubion SS, Sood R, Kapoor E. Mayo Clinic Proceedings. 2017;92(12):1842-1849. doi:10.1016/j.mayocp.2017.08.019.
Nappi RE, Martini E, Cucinella L, et al. Frontiers in Endocrinology. 2019;10:561. doi:10.3389/fendo.2019.00561.
6. Hormone Therapy for Postmenopausal Women.
Pinkerton JV. The New England Journal of Medicine. 2020;382(5):446-455. doi:10.1056/NEJMcp1714787.
7. Management of Menopausal Symptoms: A Review.
Crandall CJ, Mehta JM, Manson JE. JAMA. 2023;329(5):405-420. doi:10.1001/jama.2022.24140.
Abdelgader A, Govender M, Kumar P, Choonara YE. Journal of Pharmaceutical Sciences. 2023;112(6):1566-1585. doi:10.1016/j.xphs.2023.02.021.
9. Vagifem. FDA Drug Label.
Food and Drug Administration.
Constantine GD, Simon JA, Pickar JH, et al. Current Medical Research and Opinion. 2018;34(12):2131-2136. doi:10.1080/03007995.2018.1527578.
11.
IMVEXXY. FDA Drug Label.
Food and Drug Administration
12.
Vaginal Estrogen for Genitourinary Syndrome of Menopause: A Systematic Review.
Rahn DD, Carberry C, Sanses TV, et al. Obstetrics and Gynecology. 2014;124(6):1147-1156. doi:10.1097/AOG.0000000000000526.
13.
Mitchell CM, Reed SD, Diem S, et al. JAMA Internal Medicine. 2018;178(5):681-690. doi:10.1001/jamainternmed.2018.0116.
14.
Endometrial Safety of Low-Dose Vaginal Estrogens in Menopausal Women: A Systematic Evidence Review.
Constantine GD, Graham S, Lapane K, et al. Menopause (New York, N.Y.). 2019;26(7):800-807. doi:10.1097/GME.0000000000001315.
Endometrial Safety of Low-Dose Vaginal Estrogens.
Stanczyk FZ, Mandelbaum RS, Matharu H, Dancz CE, Sherman ME. Menopause (New York, N.Y.). 2023;30(6):650-658. doi:10.1097/GME.0000000000002177.
16.
Femring. FDA Drug Label.
Food and Drug Administration
17.
Safety of Vaginal Estrogens: A Systematic Review.
Crandall CJ, Diamant A, Santoro N. Menopause (New York, N.Y.). 2020;27(3):339-360. doi:10.1097/GME.0000000000001468.
Mitchell CM, Larson JC, Crandall CJ, et al.
JAMA Network Open. 2022;5(11):e2241743. doi:10.1001/jamanetworkopen.2022.41743.
19. Updates to Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline.
Anger JT, Bixler BR, Holmes RS, et al. The Journal of Urology. 2022;208(3):536-541. doi:10.1097/JU.0000000000002860.
Chen YY, Su TH, Lau HH. International Urogynecology Journal. 2021;32(1):17-25. doi:10.1007/s00192-020-04397-z.
21. Oestrogens for Preventing Recurrent Urinary Tract Infection in Postmenopausal Women.
Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. The Cochrane Database of Systematic Reviews. 2008;(2):CD005131. doi:10.1002/14651858.CD005131.pub2.
Brubaker L, Carberry C, Nardos R, Carter-Brooks C, Lowder JL. Female Pelvic Medicine & Reconstructive Surgery. 2018 Sep/Oct;24(5):321-335. doi:10.1097/SPV.0000000000000550.
23. Topical Estrogen Treatment Augments the Vaginal Response to Escherichia Coli Flagellin.
Stanton A, Mowbray C, Lanz M, et al. Scientific Reports. 2020;10(1):8473. doi:10.1038/s41598-020-64291-y.
24. Estrogen Supports Urothelial Defense Mechanisms.
Lüthje P, Brauner H, Ramos NL, et al. Science Translational Medicine. 2013;5(190):190ra80. doi:10.1126/scitranslmed.3005574.